Qual os métodos diagnósticos que melhor podem prever doença de Crohn em fase precoce , na qual ainda não temos complicações que sejam indicações cirúrgicas ou irreversíveis ?
Essa é uma questão que vêm sendo esclarecida com o uso da endoscopia e suas variantes ( cápsula endoscópica) que traz benefícios como classificação do Tipo de acometimento predominante ( estenos, inflamação ou fístulas ) e avaliação da resposta à terapia com medicamentos ( principalmente o Anti-TNF , embora ainda muito pouco usado no Brasil)
Assim recomendo esse artigo ( com slides para baixar) que traz imagens e texto comentando os principais achados endoscópicos da doença de Crohn.
(clique em Next para alternar entre slides)
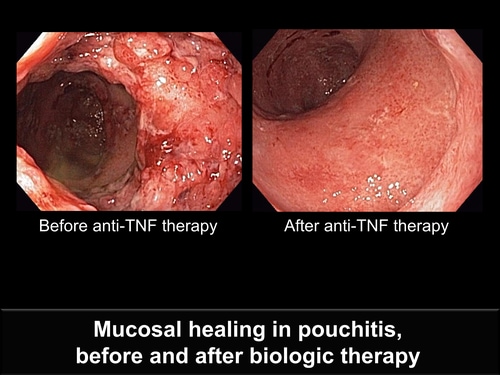
Mucosal healing has become an important endpoint of medical therapy for Crohn disease, since patients who have mucosal healing have lower rates of surgery and hospitalization than those who have no mucosal healing. Biologic agents and thiopurines are associated with mucosal healing.[1,2] Corticosteroid treatment is not associated with mucosal healing.
The image at left is an ileal pouch demonstrating extensive ulceration, pseudopolyps, edema, and friability. The image at right demonstrates mucosal healing following treatment with an anti-tumor necrosis factor (TNF) agent. The absence of mucosal ulcerations defines mucosal healing. Of note, the appearance of the mucosa is not normal; there is erythema and a distorted vascular pattern, but ulcerations, edema, and friability have disappeared with treatment. Among patients who have Crohn disease who are treated with anti-TNF agents, rates of mucosal healing are usually lower than rates of steroid-free remission.[3] Therefore, it cannot be assumed, based on symptoms, that mucosal healing has occurred. Endoscopy is necessary.
1. Rutgeerts P, Van Assche G, Sandborn WJ, et al. Adalimumab induces and maintains mucosal healing in patients with Crohn’s disease: data from the EXTEND trial. Gastroenterology. 2012;142:1102-1111.
2. Hébuterne X, Lémann M, Bouhnik Y, et al. Endoscopic improvement of mucosal lesions in patients with moderate to severe ileocolonic Crohn’s disease following treatment with certolizumab pegol. Gut. 2012. [Epub ahead of print]
3. Colombel JF, Sandborn WJ, Reinisch W, et al; SONIC Study Group. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010;362:1383-1395.
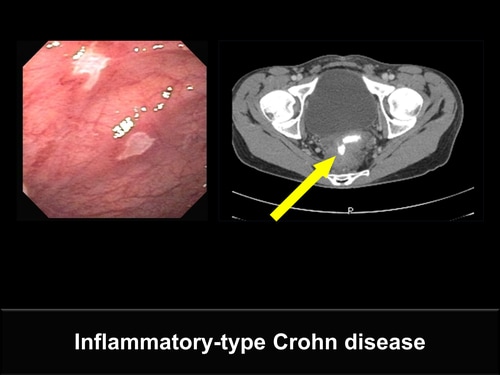
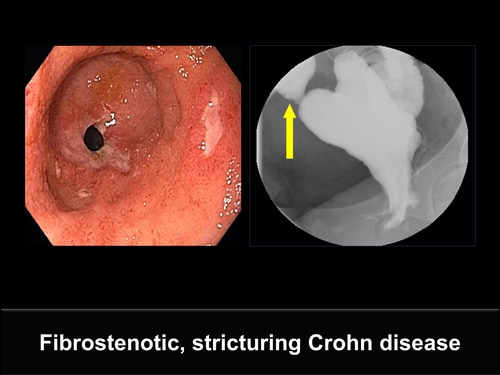
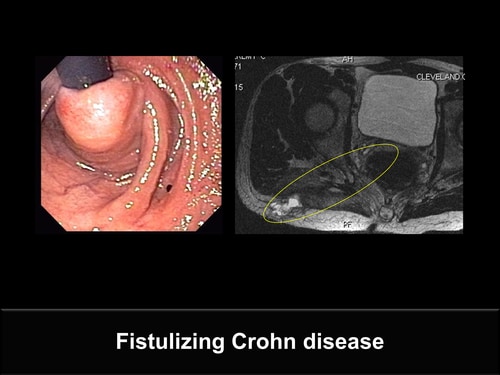
The 3 principal behaviors of Crohn disease are inflammatory, stricturing, and fistulizing disease. Early in the course of disease, most patients have inflammatory-type disease which is amenable to anti-inflammatory agents.[1] As the disease progresses, patients develop fibrostenotic stricturing-type disease and fistulizing-type disease, which are less responsive to anti-inflammatory therapy.[2]
1. Cosnes J, Cattan S, Blain A, et al. Long-term evolution of disease behavior of Crohn’s disease. Inflamm Bowel Dis. 2002;8:244-250.
2. Shen B, Remzi FH, Lavery IC, Lashner BA, Fazio VW. A proposed classification of ileal pouch disorders and associated complications after restorative proctocolectomy. Clin Gastroenterol Hepatol. 2008;6:145-158.
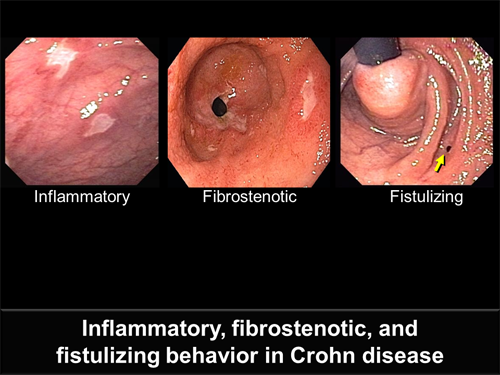
This image demonstrates a typical finding of inflammatory-type Crohn disease. The ulcers in this ileal pouch are irregularly shaped, sharply demarcated, and have intervening regions of normal mucosa (skip lesions). These are typical findings early in the course of Crohn disease that should respond to biologic agents and other anti-inflammatory therapies.
This image demonstrates an ulcerated stricture at the inlet of the ileal pouch with accompanying ulceration in the pouch itself. Although anti-inflammatory agents, such as biologic therapy, should treat the ulcerated mucosa, the fibrotic stricture will not be affected and may even worsen. Often these patients will require endoscopic balloon dilation of the stricture or surgery.
Although no inflammation is seen in this image, the arrow points to the internal os of a fistula from the ileal pouch to the gluteal region. When fistulas occur in the setting of active inflammation, biologic therapy and thiopurines are likely to help heal the fistula. With no inflammation, this patient's disease will not respond to anti-inflammatory therapy. Fibrin glue and plugs are effective in some of these patients.
Although it is thought that ileal pouches occur only in ulcerative colitis, some patients who develop an ileal pouch have undiagnosed Crohn disease. The ulcers seen in the ileal pouch are large, irregular, and have skip lesions -- all of which strongly suggest Crohn disease of the pouch. Granulomas shown on biopsy specimens of these lesions confirm the diagnosis.
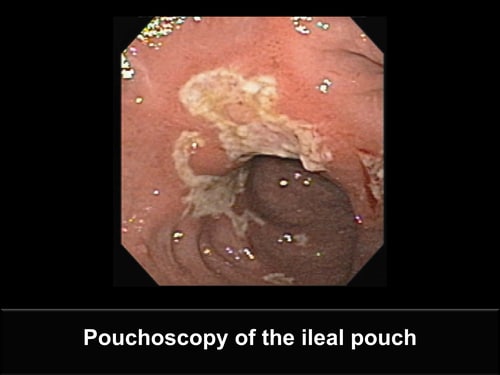
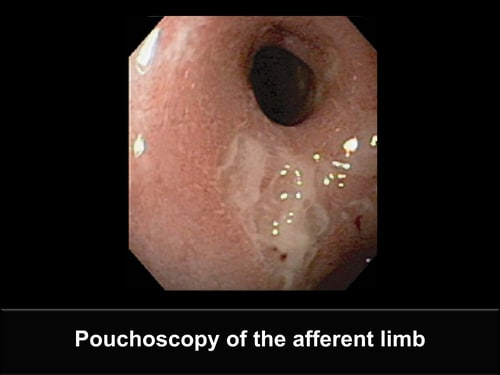
The diagnosis of Crohn disease of the ileal pouch is often very difficult. The presence of characteristic ulcers in the pouch is helpful. Biopsy results that show granulomas, pyloric gland metaplasia, lymphoid aggregates, or microscopic skip areas also may contribute to the diagnosis. An excellent marker of Crohn disease of the ileal pouch is afferent limb ulceration in the absence of NSAID use, as demonstrated in this image.
Wolf JM, Achkar JP, Lashner BA, et al. Afferent limb ulcers predict Crohn’s disease in patients with ileal pouch-anal anastomosis. Gastroenterology. 2004;126:686-9.
This ileal pouch demonstrates large, serpiginous, and longitudinal ulcerations. The intervening mucosa is less affected, but not normal. Although Crohn disease of the pouch is the principal diagnostic consideration, the differential diagnosis includes acute pouchitis, chronic pouchitis, antibiotic-associated pouchitis, and cytomegalovirus pouchitis. The clinical situation guides additional testing.
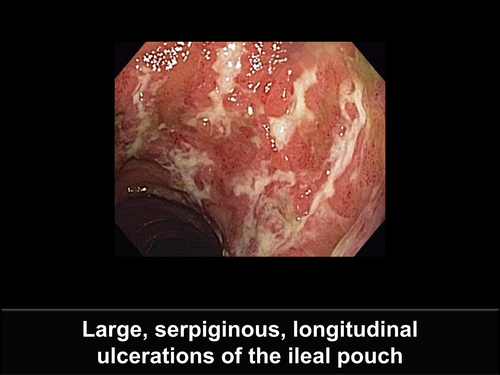
This ileal pouch demonstrates ulcerations with no intervening normal mucosa, an inlet stricture, afferent limb ulcerations, and pseudopolyps. Biopsy specimens of pseudopolyps demonstrated inflammatory changes and no dysplasia. The presence of pseudopolyps is a sign of ongoing chronic inflammation seen with Crohn disease of the pouch or chronic pouchitis. Distinguishing between Crohn disease of the pouch and chronic pouchitis can be challenging, but inlet stricture and afferent limb ulcerations suggest Crohn disease. Other features of Crohn disease are fistulas, skip lesions, and granulomas.

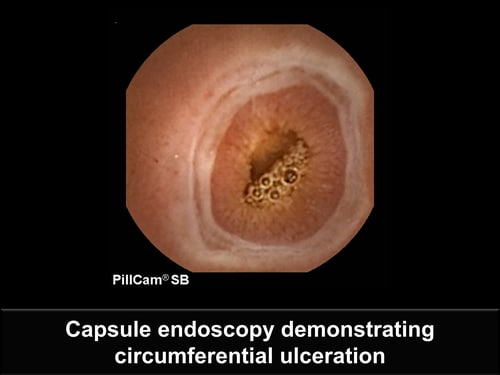
Although sensitivity of capsule endoscopy for Crohn disease is excellent, the specificity is sufficiently low that findings require corroborative testing: the diagnosis of Crohn disease cannot be made entirely by capsule endoscopy. This image demonstrates a circumferential ulceration that is not obstructing -- the capsule passed easily. Corroborative evidence to diagnose Crohn disease includes the presence of additional ulcerations in the absence of NSAID use and biopsy results demonstrating chronic inflammatory changes and/or granulomas.
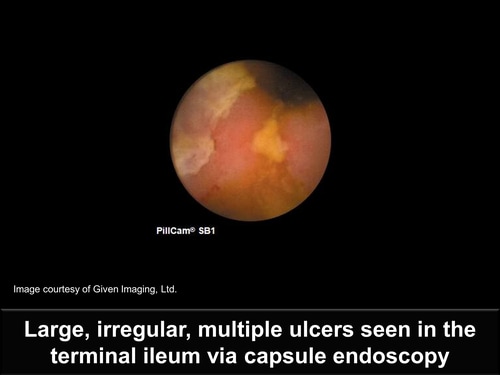
Large, irregular, multiple ulcers are apparent in the terminal ileum. There is also a suggestion of normal mucosa between ulcers. Although NSAID use and ischemic changes are included in the differential diagnosis, the proper clinical setting may allow the diagnosis of Crohn disease to be made from the capsule endoscopy findings with no corroborative testing.
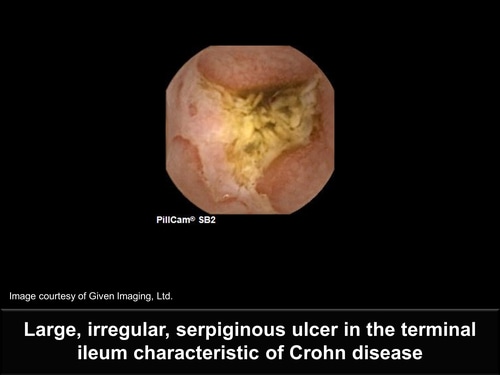
This large, irregular, serpiginous ulcer in the terminal ileum is so characteristic of Crohn disease that no corroborative evidence is needed (assuming there is no NSAID use or no patient history to suggest ischemia). The image also demonstrates retained intestinal contents at the site of ulceration, suggesting a narrowing in that area. A patency capsule or some form of small bowel imaging should be performed to rule out a stricture before capsule endoscopy is performed in patients with suspected Crohn disease.
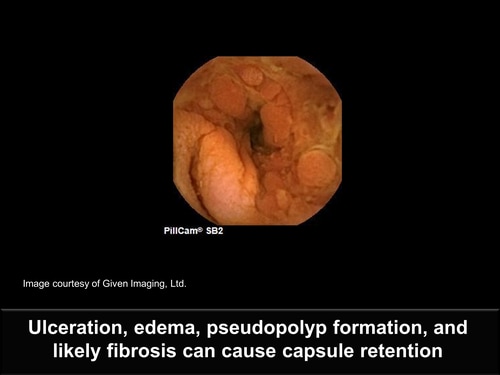
This image obtained through capsule endoscopy demonstrates characteristic findings in Crohn disease, such as ulceration, edema, pseudopolyp formation, and likely fibrosis. The capsule could not pass the stricture spontaneously. Most retained capsules do not obstruct and can be removed endoscopically -- as occurred in this case -- as long as deep enteroscopy is available. Surgical removal and resection of the affected bowel may be necessary.
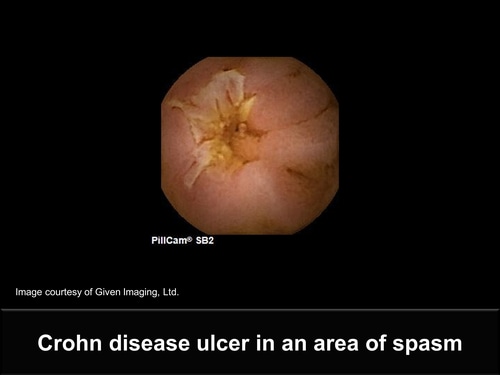
Although this image appears to suggest an irregular ulcer in an area of stricture, there was no stricture. The normal villous architecture seen beyond the ulcer suggests that this is a Crohn disease ulcer in an area of spasm. An ulcer caused by NSAID use would be circumferential, or more likely have a "kissing" ulcer on the opposite side.
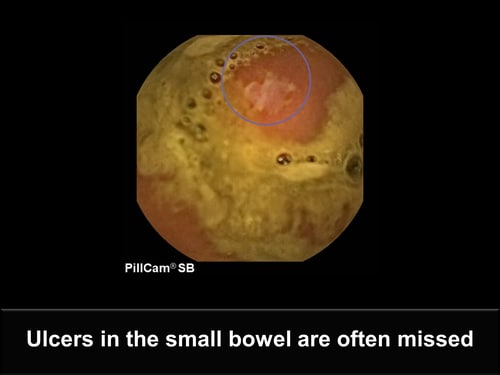
Ulcers in the small bowel may be missed due to the presence of intestinal debris or lack of attentiveness by the reader. This irregular, shallow ulcer suggesting Crohn disease was seen in only 1 image after intestinal debris cleared. It could have been easily missed. Because no other ulcerations were seen, corroborative evidence is necessary before the diagnosis of Crohn disease can be made.
This large circumferential ulcer seen in the mid-small bowel is sharply demarcated, with no mass effect, and the only abnormality seen in this patient. This is more likely an ulcer caused by NSAID use rather than Crohn disease, but a deep endoscopy will be needed with careful biopsies to make the correct diagnosis.

-->
'via Blog this'